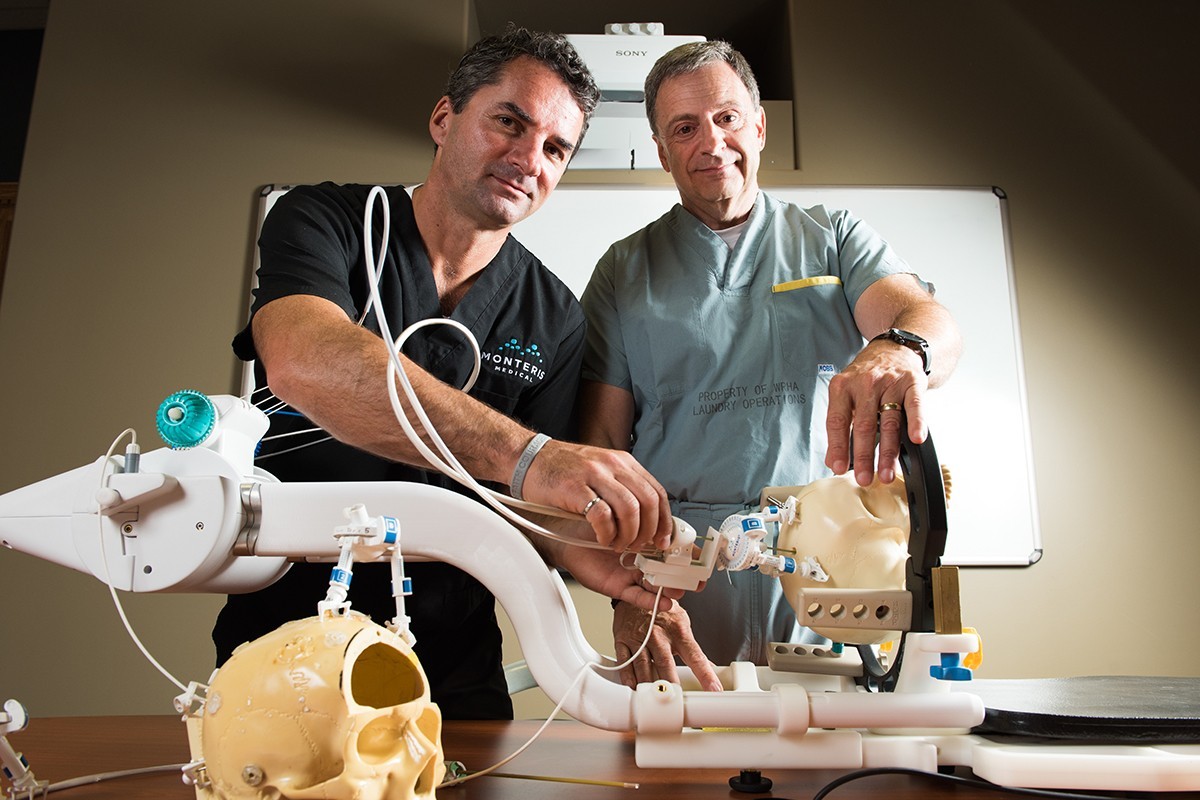
Alumni Richard Tyc [MSc/94] and Dr. Mark Torchia [PhD/01] with the NeuroBlate® System
It’s still brain surgery, but it’s been made slightly easier
Made-in-Manitoba technology gives surgeons non-invasive access to the inner parts of the brain, saving lives and transforming the hospitals of the future
Surgeons can now destroy previously inoperable tumors deep inside the brain using a revolutionary tool developed by two investigators at the St-Boniface Hospital Albrechtsen Research Centre, for which they received the 2015 Ernest C. Manning Principal Award.
University of Manitoba Alumni Dr. Mark Torchia [PhD/01] and Richard Tyc [MSc/94] are receiving the award for their joint development of the NeuroBlate® System. Torchia is currently an associate professor of surgery in the U of M’s College of Medicine and the director of the University’s Centre for the Advancement of Teaching and Learning. Tyc is vice-president, technology and advanced technology, at Monteris Medical, a spinoff company established in 1999 to create groundbreaking neurosurgical technologies.
“This award represents years of persistence, a true bench-to-bedside success story,” says Dr Grant Pierce, St-Boniface Hospital executive director of research. “This is a proud moment for the St-Boniface Hospital Foundation, which supported this project from its inception to prototype development.”
The award announcement was made today at the University of Saskatchewan and the inventors will receive their $100,000 award at a gala tomorrow in Saskatoon.
The NeuroBlate System is a unique technology that allows surgeons to treat otherwise inoperable brain tumors that reside deep in the brain’s tissue. Surgeons begin by drilling a hole in the skull about the size of a pencil. They insert the Monteris NeuroBlate® System MRI-guided laser probe and use real-time data to guide the probe through the brain to the tumor. There, the surgeons can put the probe into the cancerous mass and destroy it from the inside out with a laser. Essentially, this new tool allows surgeons to cook the tumor with lethal heat that they can control with unprecedented ability. The tumor is destroyed and the healthy surrounding tissue is preserved. It is the only system in the world that allows surgeons to see the tumor in 3-D, providing them with critical information they need to make treatment decisions in the operating room.
“We are extremely proud of our outstanding alumni and congratulate them on this well-deserved national award,” says Dr. David T. Barnard, president and vice-chancellor of the University of Manitoba. “Their life-saving technology is having a global impact and Manitobans should be proud of the tremendous work being done at the St-Boniface Hospital Albrechtsen Research Centre, the University’s long-time research partner.”
University of Manitoba professors last won a Manning Principal Award in 2010: Professor Werner Ens and Ken Standing were recognized for their work in the field of mass spectrometry that has profoundly shaped drug development, disease studies and agriculture.
About the Award
Since 1982, The Ernest C. Manning Awards Foundation has been creating a culture of innovation in Canada by discovering, celebrating and rewarding Canadian innovators of all ages. We tell the stories of Canadian innovators who are improving the lives of Canadians and others around the world through their commercialized innovations.
Research at the University of Manitoba is partially supported by funding from the Government of Canada Research Support Fund.








Congratulations on this achievement! Brain cancer is a horrible disease. It cut the life of a very good friend of mine.
I am very happy to see this type of innovation! Great work! And thank you!
Good work, but this will only debulk the tumor and not destroy the invasive cells which almost always cause recurrence. We need a better way to identify and eliminate invading cells in addition to the bulk tumor