Breastfeeding is recommended during pandemic, but coronavirus has changed support systems
Breastfeeding sets babies up for good health across the lifespan. However, the COVID-19 pandemic is causing health-care providers to change the way they support breastfeeding mothers. While many supports have been reduced or eliminated, others have transitioned online where it may be easier for families to access them.
As researchers in the field of breastfeeding and human lactation, we are asking many questions about the safety of breast milk from mothers who are sick with COVID-19, the impact of COVID-19 on quality of care and breastfeeding support, and how the pandemic will affect breastfeeding rates.
Is it safe to breastfeed my baby during COVID-19?
The Public Health Agency of Canada and the Canadian Pediatric Society recommend that mothers suspected of or confirmed positive for COVID-19 continue to breastfeed. Currently, there is no evidence of the presence of the SARS-CoV-2 virus in breast milk. This means that breast milk itself is likely not a potential route for transmission of COVID-19.
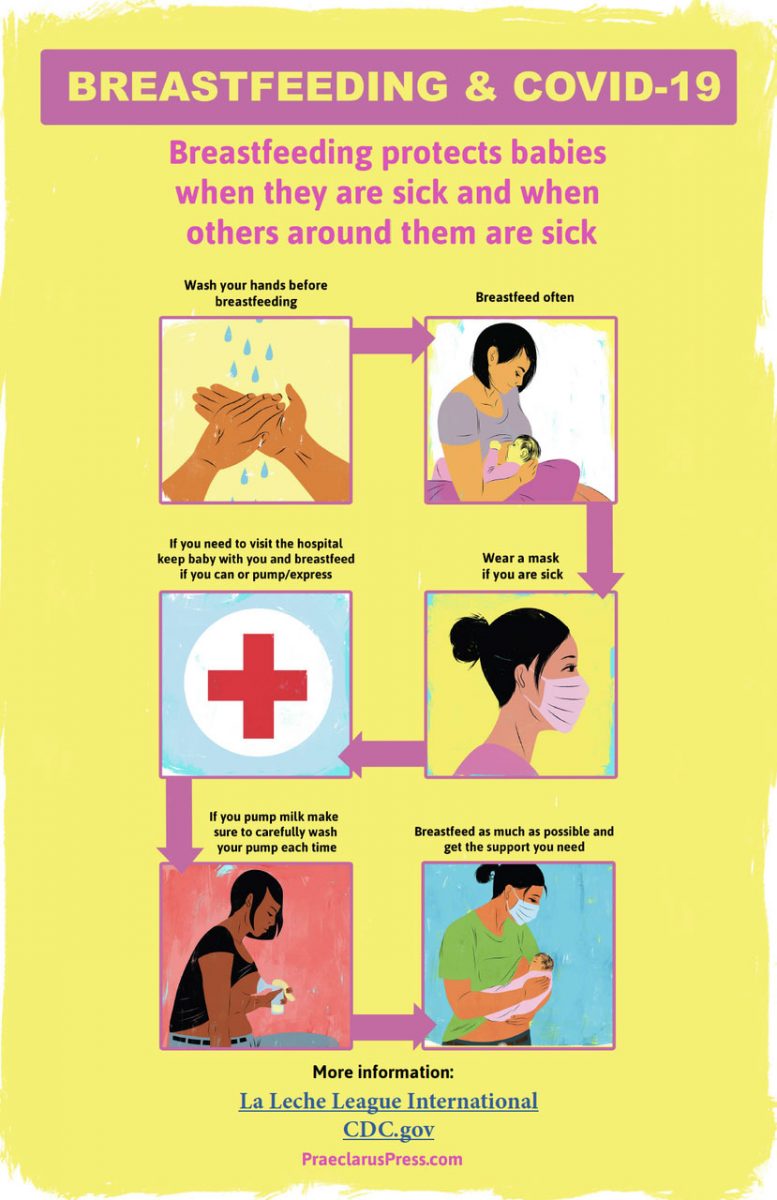
COVID-19 is primarily spread through droplets, which could be a path for transmission from a sick mother to her baby. However, there are many benefits of breastfeeding including providing antibodies that contribute to strong immune system development.
Current recommendations state that sick mothers can remain with their infant and continue to breastfeed while taking extra precautions. These include wearing a mask, washing hands frequently and disinfecting surfaces that may be in contact with the infant. Pumping breast milk and feeding the infant from a cleaned bottle is recommended for mothers who are too sick to feed at the breast.
If a mother is not sick, they can continue to breastfeed the way they normally would.
Establishing breastfeeding requires significant professional and social supports. In the midst of the COVID-19 pandemic, practitioners are grappling with how to best support breastfeeding mothers in safe and healthy ways.
The current evidence on the extent to which COVID-19 affects moms and babies is preliminary and still ongoing. That means families and practitioners may have to deal with changing recommendations and information about COVID-19, which may bring about disruptions in care. Health-care agencies are choosing to use the precautionary principle, which favours stricter regulations than may be necessary.
How have breastfeeding supports changed?
Breastfeeding support is critically important in helping moms continue to breastfeed and meet their own breastfeeding goals. There are approximately 1,000 babies born each day in Canada, 89 per cent of whom begin breastfeeding in hospital.
However, many maternity care centres are now discharging families with uncomplicated deliveries six hours after birth. This means that there is currently very little breastfeeding support available in hospital and the responsibility has shifted to care in the community.
Community breastfeeding supports have also changed in light of COVID-19 restrictions. Practitioners who work in clinics helping mothers with breastfeeding issues have seen a decrease in in-person assessments due to families wanting to stay at home. In-person breastfeeding assessments are important because practitioners can assess latch and tongue tie, and help with positioning. Further, many health regions have discontinued their prenatal and breastfeeding classes.
On the other hand, there has been a surge in virtual and phone-based assessments, which were not available to families prior to COVID-19. Virtual formats for breastfeeding support can reach more families in the safety of their own homes.
Professional breastfeeding support is important, but so is social support. Due to social distancing measures, in-person breastfeeding support groups have been cancelled and visits from friends and family members are off limits. Social support can improve mothers’ confidence and success (what researchers call self-efficacy) in breastfeeding and provide the emotional stamina to continue on. The importance of professional and social supports on the initiation and duration of breastfeeding are well supported and the impact of COVID-19 on breastfeeding outcomes could be significant.
What are the new opportunities for breastfeeding mothers?
Among the new barriers present for breastfeeding mothers, there are also breakthroughs. These breakthroughs may provide better support to previously unreached populations. COVID-19 has forced providers to transition to online care, which can offer services to women and families in remote locations.
Through online platforms, providers can also see women in their own homes and offer tailored recommendations based on their current set-up. In many areas, there are now online parenting support groups and online videos are being created to provide pre- and post-natal care to families.
Additionally, while tangible social supports from friends and family are reduced, there are benefits to mothers having uninterrupted time with their infants, which can help to enhance the breastfeeding relationship.
Our current circumstances are shifting the way breastfeeding support is provided. Looking ahead, we see great opportunities to merge new online support systems with in-person supports to provide more options and better care to new babies and families.
This story from Merilee Brockway, Post-doctoral Fellow, department of Pediatrics and Child Health, UM, and also at the Children’s Hospital Research Institute of Manitoba, and Sarah Turner, PhD candidate, Community Health Sciences, UM, and at the Children’s Hospital Research Institute of Manitoba, was published online by The Conversation.
Research at the University of Manitoba is partially supported by funding from the Government of Canada Research Support Fund.