Measuring the mental health of military members
A new series of studies looking into the mental health of Canadian Armed Forces members aims to better understand the connections between mental health and military service.
The studies follow up with data collected by Statistics Canada in collaboration with the Department of National Defence in 2002 and compare it with more recent data from 2018. In 2002 participants were asked to fill out a survey on mental health. In 2018 researchers contacted 2,941 of the original 5,155 participants and asked them to fill out the survey again. The survey aims to show clinicians and stakeholders how mental health changes after 16 years of service in the military.
“We figured it was important to follow up with some of these people and see how their mental health changed over their service. This is an important gap in the literature right now,” says Dr. Shay-Lee Bolton, assistant professor of psychiatry, Max Rady College of Medicine, Rady Faculty of Health Sciences. “Seeing people at one-time point and then comparing with another to see what is changed and the same hasn’t been done before.”
In every category including anxiety, depression and PTSD, there is an increase in the number of people who have been diagnosed with a disorder. Bolton isn’t yet sure yet why there has been an increase in diagnoses but recognizes that it’s something to keep an eye on.
“I think it shows a vulnerability that’s there. We don’t know that it’s due to their military experience, but it shows that there is a vulnerable population there,” says Bolton.
The studies found that there were risk factors and protective factors when it came to avoiding and dealing with PTSD and major depressive disorder. Some of the risk factors for developing PTSD or major depressive disorder include: being female, being involved in land operations, having other mental health issues or being a junior non-commissioned officer. Participants were less likely to develop major depressive order or PTSD if they had access to bolstered social supports, social networks and problem-focused coping strategies.
“I think some of the key features of these studies are knowing what those predictors of mental health are 16 years later,” says Bolton.
She hopes that this information will be helpful for people with these risk factors, so they may seek out mental health services during their service or beforehand.
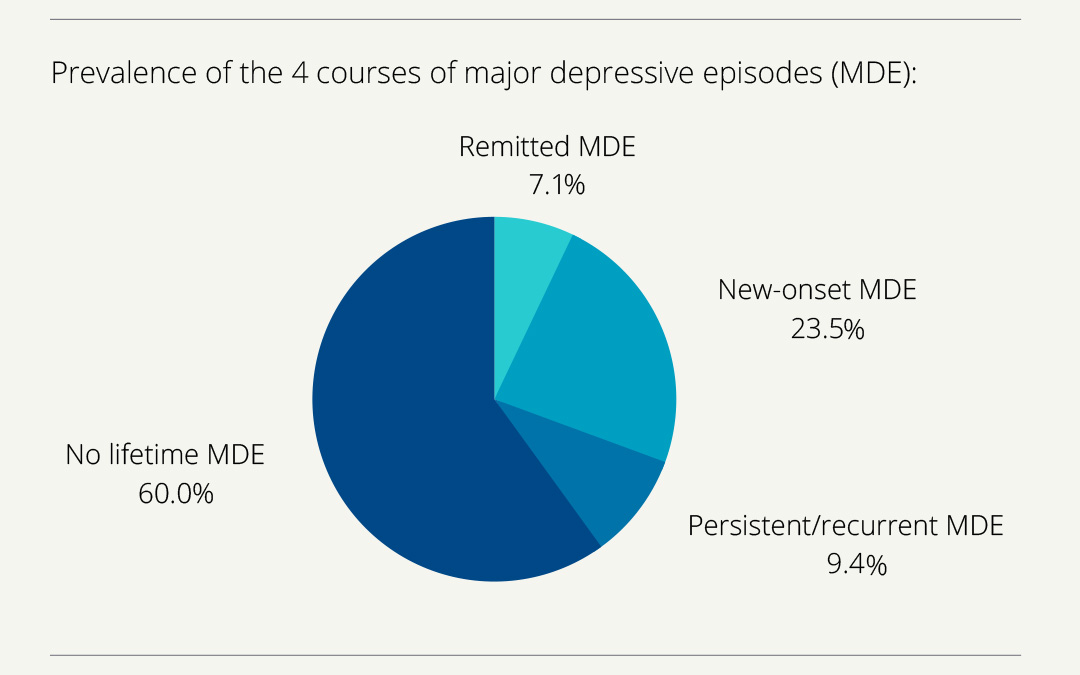
To share this information, researchers created four easily accessible infographics with the main findings of each study. Hopefully, Bolton says, this will make the information easy to understand.
“It’s a real chance for us to display the work in this cohesive way. It’s an easy way for individuals to be able to access and learn what the study has taught us,” she says. “We want this [information] to be broadly applicable for members of the armed forces and the general public. Research articles are generally harder to access and to read. The infographics make the main messages clear.”
While some of the findings are startling, Bolton hopes that the research she and her team have been working on will be able to make a difference in the lives of those serving.
“Research is exciting. It highlights all the places we need to put in effort and work and perhaps finance in terms of changing things for the better for people’s mental health.”






