
Inside the virtual reality setting that Dr. Renée El-Gabalawy and her team are using to treat phantom limb pain.
The Winnipeg Foundation Innovation Fund supports cutting-edge projects
Three interdisciplinary teams from the Rady Faculty of Health Sciences have received $100,000 grants from The Winnipeg Foundation Innovation Fund to pursue leading-edge research in the areas of heart disease, phantom limb pain and Huntington’s disease.
The one-year grants are part of The Winnipeg Foundation’s $1-million commitment to support innovative medical research projects at the University of Manitoba.
“The goal of this fund is to bring together cross-disciplinary teams to help launch exciting and innovative research,” says Dr. Jude Uzonna, vice-dean, research, Rady Faculty of Health Sciences. “These three projects are excellent examples of the cutting-edge work taking place at the Rady Faculty and the type of research that can be accomplished when we bring together experts from different fields.”
Virtual reality phantom limb pain treatment
A team led by Dr. Renée El-Gabalawy, associate professor of clinical health psychology, and anesthesiology, perioperative and pain medicine at the Max Rady College of Medicine, is using virtual reality (VR) to treat phantom limb pain. The condition, which typically does not respond to standard pain treatments, causes the perception of painful sensations like stabbing, burning or throbbing in a limb that has been amputated.

Dr. Renée El-Gabalawy
The team will be building on its previous research that developed VR technology that incorporated graded motor imagery, a technique used to treat chronic pain by retraining the brain. They will also be conducting a clinical trial to evaluate whether the first-of-its-kind VR treatment works.
One stage of graded motor imagery uses an adapted mirror box therapy, in which a patient’s limb is simulated to make it look like their missing limb is there. This helps the brain accommodate the missing limb thereby reducing pain signals. In the VR setting, the patient sees themself with both their limbs as they perform a sequence of exercises with the use of integrated sensor technology.
“This funding is instrumental in terms of taking our research to the next step,” El-Gabalawy said. “If it’s found to be effective, I envision a future where this VR treatment will not only be accessible to patients in the hospital, but also in the comfort of their homes.”
Co-principal investigators include Dr. David Perrin, assistant professor of orthopedic surgery, and Dr. Justin March, assistant professor of internal medicine, Max Rady College of Medicine, and Dr. Elizabeth Hammond, assistant professor of physical therapy, College of Rehabilitation Sciences.
Team studies Huntington’s disease
Dr. Galen Wright, UM Canada Research Chair in neurogenomics, and assistant professor of pharmacology and therapeutics, and biochemistry and medical genetics, at the Max Rady College of Medicine, heads a project to study the genetic modifiers in Huntington’s disease, an inherited condition that causes the breakdown of nerve cells in the brain.
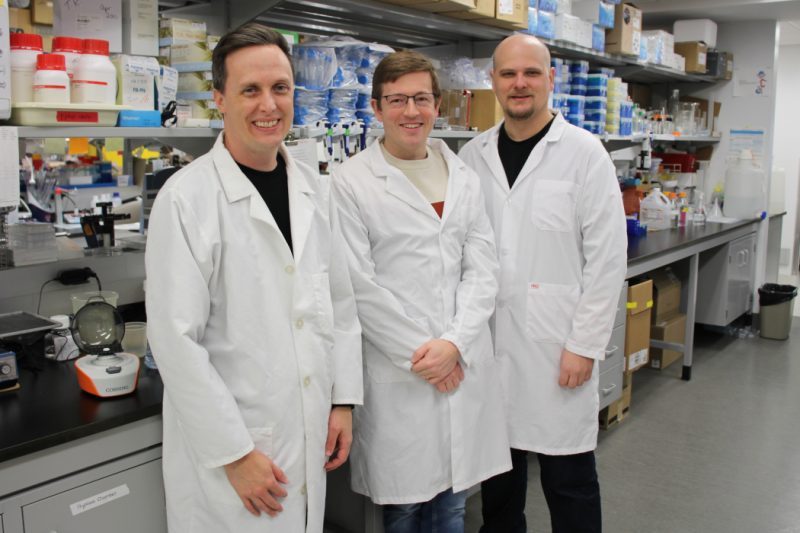
[From left to right] Dr. Galen Wright, Dr. Robert Beattie and Dr. Paul Marcogliese.
“Even though we have known the genetic cause of Huntington’s disease for more than 30 years, no effective treatments exist,” Wright said. “This research is innovative because many of the technologies we are using only became available in recent years.”
The team – comprising experts in human genetics and neuroscience – will take a multifaceted approach throughout this study. The researchers will use innovative techniques to monitor the progression of individual brain cells in animal models. They will also employ an advanced genomic technique, single-cell sequencing, to look at gene expression changes in cell types to understand what’s going on at the disease level.
Wright said Huntington’s disease is among a group of more than 50 diseases caused by genetic mutations known as repeat expansions and most affect the brain. What the team learns from this project could be useful in developing drugs to treat all those diseases, he says.
Co-principal investigators from the Max Rady College of Medicine include Dr. Robert Beattie, assistant professor of biochemistry and medical genetics, and Children’s Hospital Research Institute of Manitoba (CHRIM) researcher, and Dr. Paul Marcogliese, assistant professor of biochemistry and medical genetics, and CHRIM researcher.
Using multi-omics and artificial intelligence to study heart disease
A study led by Dr. René Zahedi, professor of internal medicine, and biochemistry and medical genetics at the Max Rady College of Medicine, is using multi-omics and artificial intelligence to help better understand calcified aortic valve stenosis. The disease occurs when the heart valve to the main artery doesn’t fully open, resulting in a reduction of blood flow to the body.
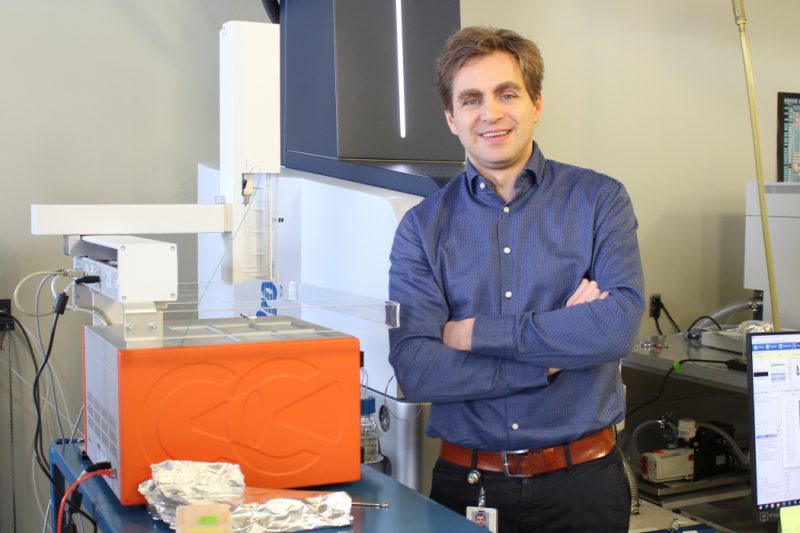
Dr. René Zahedi
“Calcified aortic valve stenosis is the third leading cause of adult heart disease and we don’t really know what’s causing it,” Zahedi said. “The disease has a very complex molecular mechanism, so we want to look at the disease from different perspectives.”
Team members will use their expertise in proteins and lipids to look at what is going wrong in the heart valve on a molecular level and how it can be treated or stopped. They will also work to identify markers in the blood that could detect early stages of the disease or whether someone will develop it.
Zahedi said the cutting-edge aspect of this research will be their use of artificial intelligence to analyze the data. If all goes well, he said the approach they’re taking in this study could be applied in other areas like cancer and chronic disease research.
Co-principal investigators include Dr. Amir Ravandi, associate professor of internal medicine, and physiology and pathophysiology, and Dr. Richard LeDuc, associate professor of biochemistry and medical genetics and director of bioinformatics at CHRIM, from the Max Rady College of Medicine.






