Family medicine holds key to healing health-care system, journalist tells UM gala audience
What’s wrong with health care?
“We’re trying to deliver 21st-century care with a 1950s model of health-care delivery and funding,” says André Picard. “We have an Edsel, but we need a Tesla.”
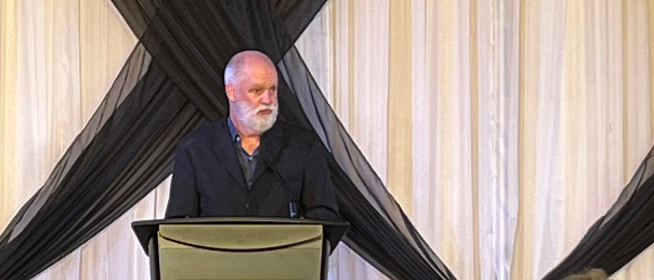
Picard, the award-winning health reporter and columnist for The Globe and Mail who is also a bestselling author in the health field, was the guest speaker at a UM gala on May 26 at the Manitoba Museum.
The celebration was held to mark the 50th anniversary of the 1973 founding of the department of family medicine in what is now the Max Rady College of Medicine.
Picard, whose honours include being named Canada’s first Public Health Hero by the Canadian Public Health Association, addressed more than 340 primary health-care providers, educators and guests at the gathering.
The medical system emphasizes sickness care, not health care, Picard said, and as far back as he can remember, it has lurched from crisis to crisis.
“The pandemic didn’t break the health-care system,” he said. “It was already broken.”
Results from the 2022 OurCare national survey estimate that more than one in five Canadian adults – 6.5 million people – do not have a family physician or nurse practitioner they can see regularly for care. Emergency departments are overflowing or closing, and it can take months or years to see a specialist.
In Picard’s view, hope lies in strengthening the all-important primary level of care. “I believe the future of medicine belongs to family medicine,” he said.
Other speakers at the gala described how UM is working hard to be part of this solution. Family medicine – already one of the largest departments in the Max Rady College of Medicine – recently went the extra mile to create an additional 10 residency spaces.
“We reached out to challenge you to say, ‘Who could you take on? What could you do?’” said Dr. Peter Nickerson, vice-dean (health sciences) and dean of the Rady Faculty of Health Sciences. “You did this in the context of coming out of the pandemic, overwhelmed. And yet you still stood up and said, ‘We’ll take more.’”
Manitoba was one of only two provinces that filled all its family medicine residency seats, including the newly created ones, in 2023. “I applaud the department of family medicine for being an integral partner in helping to ensure Manitoba’s strong health-care workforce,” said Health Minister Audrey Gordon.
Dr. José François, head of the department and provincial specialty lead, family medicine, at Shared Health, told the audience, “I strongly believe our department will play an important role in building – and rebuilding – our workforce.
“Over the past 50 years, we’ve had a great track record of stepping up. We’ve demonstrated our ability to provide continuity of care, to build meaningful relationships with patients and families, and [to make] an impact on the health and well-being of our communities.”
The UM department has been a pioneer in rural education for family doctors, François noted. “We established the Parkland residency program 25 years ago,” he said. “It was the first rural residency in the country.”
While the department is based on UM’s Bannatyne campus, over its 50 years the program has grown to include 13 training sites, serving patients as far north as Churchill and as far south as Morden, with Iqaluit to the east and Hay River, N.W.T. to the west.
In 2018, Dr. Mandy Buss, a 2011 graduate of family medicine’s northern remote stream, was named the first Indigenous health lead for the department. She is helping to guide the next generation of practitioners to ensure cultural safety for Indigenous patients and to work toward reconciliation.
The department has embraced and advanced team-based care through initiatives such as bringing the master of physician assistant studies (MPAS) program under its umbrella. François described MPAS as Canada’s leading physician assistant program.
Some of the department’s latest advances include new programming in its enhanced skills program, with a focus on addressing the addictions crisis. Two new professorships in research are working toward leading-edge quality improvement for residents. And a newly launched peer-support program is underway to combat physician burnout.
“I want to commend all the UM faculty … who play a pivotal role in providing primary care in their communities while serving as teachers and mentors, educating and training the next generation of family physicians,” said Nickerson.
“Everything we learned during the pandemic – like adaptability and fortitude – as faculty members, clinicians, learners, stayed with us. Indeed, it made us even stronger and more resilient.”






