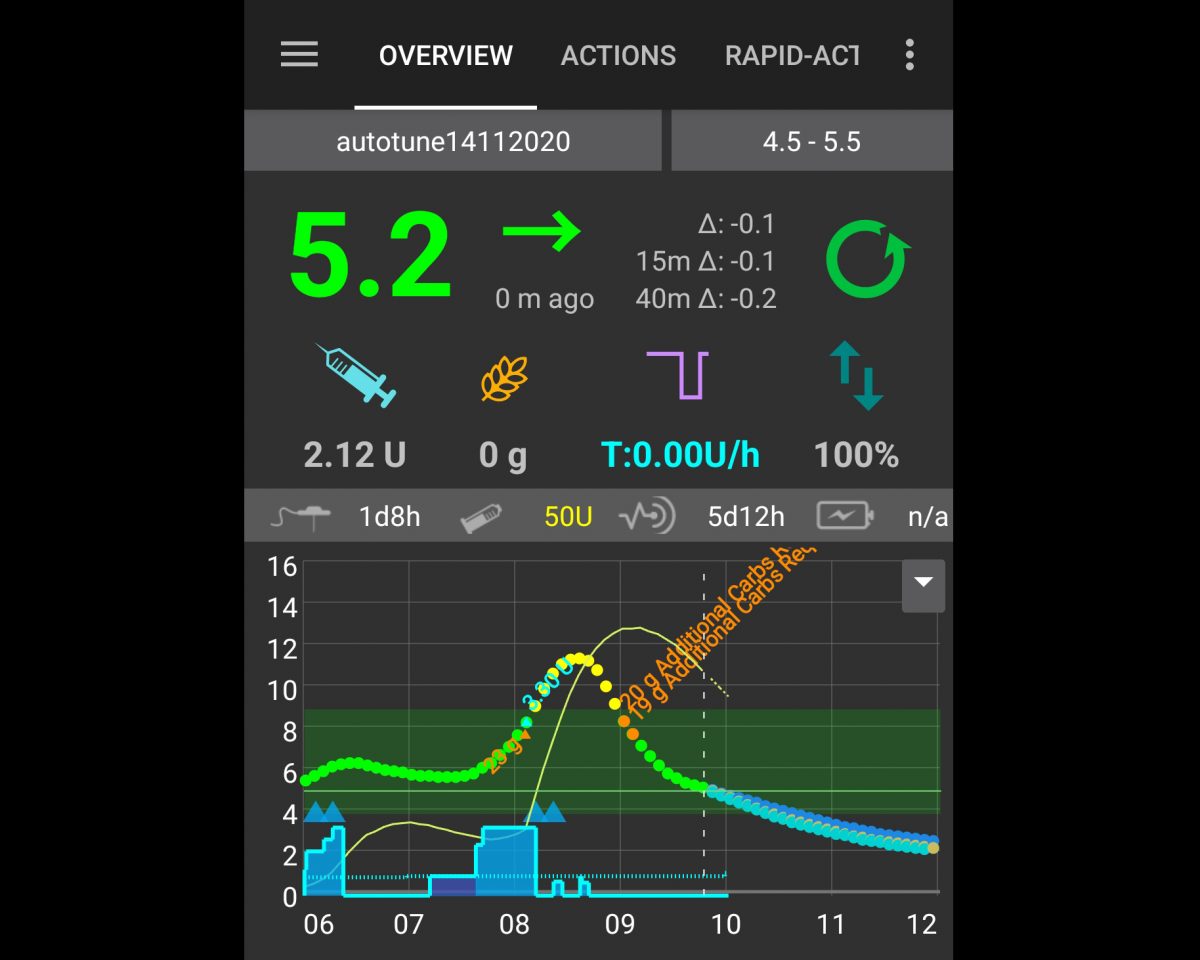
Screen-capture of Android Artificial Pancreas System closed loop system on a cell phone. Credit Dylan MacKay.
Winnipeg Free Press: It’s time Canada funded advanced diabetes treatment
The following is an op-ed written by Dylan MacKay, assistant professor of nutrition and chronic disease in the Department of Food and Human Nutritional Sciences and the Department of Internal Medicine’s endocrinology section. It was originally published in the Winnipeg Free Press on December 3, 2022.
It’s been 101 years since the discovery of insulin made survival as a person with Type 1 diabetes possible. It’s also the best time in history to be someone with Type 1 diabetes — but only if you can afford the technology. Few in Canada can or are covered for costs through public or private plans. I’m one of the lucky ones.
Even before I wake up, my blood sugar is being measured while I sleep, and the results are sent to my phone where software can warn me if my blood sugar is out of range. Even better, the closed loop pump algorithm on my phone can make changes to the amount of insulin I’m getting from my insulin pump, to prevent my blood sugars from going out of range.
The best part is I can sleep through the whole process and get up rested and well.
This technology is made possible by the development of continuous glucose monitors (CGM). CGM are wearable devices that track your blood sugar every few minutes, day and night. This technology has changed my life and the lives of countless others with Type 1 diabetes and their caregivers.
Before CGM, measuring blood sugar involved sticking your fingertips with a sharp piece of metal to get blood and putting the blood on a strip in a machine called a glucometer. It sucks, fingertips are sensitive, and you have sore fingertips all day, every day. You also tend to only check your blood sugar levels a few times a day.
Managing blood sugars for someone with Type 1 diabetes is a little like steering a big ship — you need to make changes in direction well before they need to happen, or you crash. Glucometers are like steering the ship with your eyes closed; CGM opens your eyes.
Knowing your blood sugar level and where it is going is very important, because while insulin is a wonder drug that keeps me alive, it is also incredibly dangerous.
Every time you take insulin, you put yourself at risk of low blood sugar or hypoglycemia, which is a common cause of emergency room visits for those with Type 1 diabetes. If untreated, it can kill.
CGM use has been shown to be very effective at reducing time with low blood sugar. The flip side of low blood sugar is high blood sugar, which long-term is associated with poor outcomes such a heart attacks and kidney disease. CGM helps with this as well, increasing the time that those with Type 1 diabetes have their blood sugars in a safe range.
Unfortunately, CGM costs between $3000 to $6000 a year. Most provincial/territorial health and drug plans do not cover the expense. The few that do, often have age restrictions. For instance, Manitoba has coverage for CGM, but only to those under age 25.
But people with Type 1 diabetes get old too – so where does that leave them for the rest of their lives?
Many private insurance plans also do not cover CGM. I work full-time as a University professor and CGM is not covered by our plan. Fortunately, I am lucky enough to be able to afford the out-of-pocket costs.
Without coverage, CGM simply costs too much for most Canadians with Type 1 diabetes.
Right now, the Yukon is the only place in Canada that gets coverage right. They cover CGM for everyone with Type 1 diabetes, and I bet they will be rewarded with fewer emergency room visits, lower long-term costs related to Type 1 diabetes care, and happier, healthier and more productive people.
The federal government’s long promised pharmacare plan has so far amounted to words and no action – and no guarantee CGM will be included should it ever materialize.
In the meantime, the other jurisdictions in Canada need to follow Yukon’s lead. If the provinces/territories worked together, the costs for CGM would come down and everyone in Canada would benefit.
Dylan MacKay lives with Type 1 diabetes and is an Assistant Professor of Nutrition and Chronic Disease at the University of Manitoba.






