
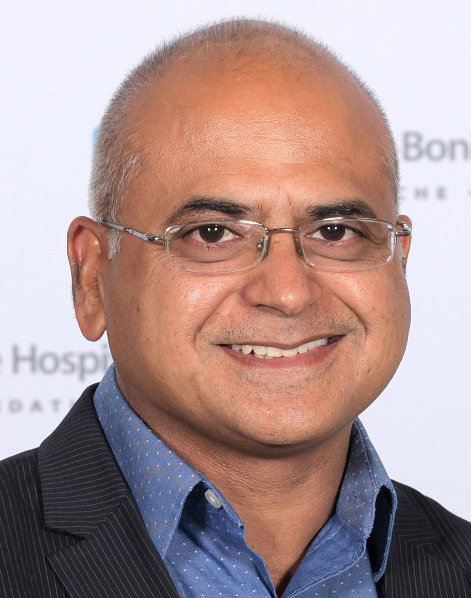
Dr. Jude Uzonna received a CIHR project grant to better understand a parasitic disease called leishmaniasis.
Rady Faculty scientists receive nearly $10 million in CIHR funding
Researchers from the Rady Faculty of Health Sciences have been awarded more than $9.9 million in the latest round of Canadian Institutes of Health Research (CIHR) project funding.
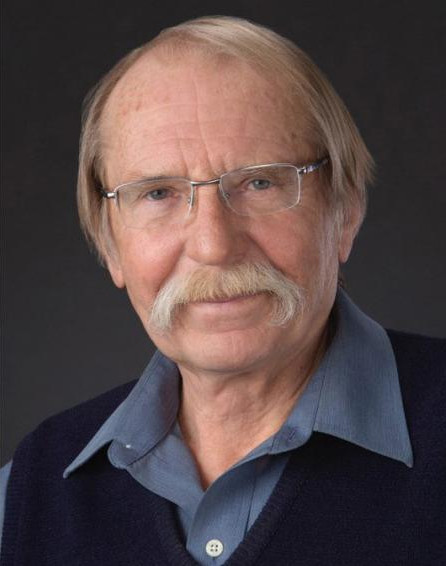
“I congratulate these successful Rady Faculty researchers and their partner networks whose work is contributing to the highest attainable standard of health as a fundamental right here in Manitoba and around the world,” said Dr. Mario Pinto, UM’s vice-president (research and international).
“It is wonderful to see Manitoba leading the nation with the highest average and median grant values, a testament to the outstanding quality of research conducted at the University of Manitoba.”
Dr. Peter Nickerson, vice-provost (health sciences) and dean of the Rady Faculty of Health Sciences, said that the funded projects in the Spring 2024 competition show the diversity of health research taking place across the faculty.
“The researchers are examining a wide range of topics – from new drug combinations to treat blood cancer to determining how the communication between astrocytes and neurons occurs. This CIHR funding is crucial for advancing science and will inevitably have an impact on the health of patients both locally and globally,” Nickerson said.
One of the 11 Rady Faculty grant recipients is Dr. Jude Uzonna, professor of immunology at the Max Rady College of Medicine and vice-dean (research) at the Rady Faculty of Health Sciences. He and his team received $1,005,976 over five years to study what could one day lead to new treatments for leishmaniasis.
Leishmaniasis is an understudied parasitic disease spread by sand flies that can cause skin sores and even fatal damage to internal organs. The disease affects more than 12 million people worldwide, Uzonna said, and it’s starting to spread to non-endemic countries like Canada.
“It’s coming,” he said. “It’s really coming because of global warming, increased immigration from endemic countries to Canada and soldiers coming back from peacekeeping duties. The numbers are growing, but if we can develop a vaccine for it, then it becomes a magic bullet used to prevent it.”
The team has found that leishmaniasis triggers the production of a molecule called pentraxin 3 (PTX3) in infected people. PTX3 weakens a specific part of the immune system that normally helps fight the parasite, so Uzonna suggests that targeting PTX3 might be a good way to develop new treatments for the disease.
This study aims to better understand the role of PTX3 in the disease. It will also look at whether the level of PTX3 can predict if someone will benefit from treatment or not, which is important because the current drugs used can be toxic.
“If we can show that PTX3 is causing a problem, then we can develop a molecule that can target and block PTX3 production. We can combine the molecule with a drug to make treatment more efficient and better. That will have a significant impact,” Uzonna said.
Rady Faculty of Health Sciences CIHR project funding recipients
 Dr. Marissa Becker, professor of community health sciences, Max Rady College of Medicine
Dr. Marissa Becker, professor of community health sciences, Max Rady College of Medicine
Grant: $100,000 (one year)
Using a program science approach, Becker and the team will develop a deeper understanding of how physical, organizational, social and relational dimensions of place shape ecologies of risk and safety for adolescent girls and young women, female sex workers and their male sexual partners in Nairobi County, Kenya. This work will generate contextualized knowledge for prioritizing place-based strategies to optimize sexually transmitted and blood-borne infection prevention program coverage and address unmet needs.
 Dr. Sanjiv Dhingra, professor of physiology and pathophysiology, Max Rady College of Medicine; researcher, Institute of Cardiovascular Sciences, St. Boniface Hospital Research Centre
Dr. Sanjiv Dhingra, professor of physiology and pathophysiology, Max Rady College of Medicine; researcher, Institute of Cardiovascular Sciences, St. Boniface Hospital Research Centre
Grant: $1,067,176 (five years)
Dhingra will lead a study focused on understanding the reasons for rejecting transplanted donor-derived mesenchymal stem cells in the heart. This research will help to develop strategies to prevent rejection and improve the survival of implanted stem cells in the heart.
 Dr. Jody Haigh, professor of pharmacology and therapeutics, Max Rady College of Medicine; researcher, Research Institute in Oncology and hematology, CancerCare Manitoba
Dr. Jody Haigh, professor of pharmacology and therapeutics, Max Rady College of Medicine; researcher, Research Institute in Oncology and hematology, CancerCare Manitoba
Grant: $1,071,000 (five years)
Haigh aims to identify new drug combinations to treat aggressive forms of blood cancer and to determine ways to avoid drug resistance to these treatments that can sometimes occur during cancer therapy. This project will be important in identifying and confirming new drug approaches that can be used in personalized medical care for childhood and adult blood cancer patients in Canada.
 Dr. Julie Lajoie, assistant professor of medical microbiology and infectious diseases, and Francis A. Plummer Professorship in Global Infectious Diseases, Max Rady College of Medicine
Dr. Julie Lajoie, assistant professor of medical microbiology and infectious diseases, and Francis A. Plummer Professorship in Global Infectious Diseases, Max Rady College of Medicine
Grant: $1,132,200 (five years)
Lajoie and the team will follow female sex workers from Nairobi, Kenya, who are using an injectable contraception called depot medroxyprogesterone acetate (DMPA) for six months and determine the immune activation and inflammatory profile in the blood and at the female genital tract. They will also examine whether using DMPA impacts the capacity to respond to previously exposed viruses and affects the cells’ capacity to respond to the stress hormone cortisol.
 Dr. Aaron Marshall, department head and professor of immunology, Max Rady College of Medicine; researcher, Research Institute in Oncology and Hematology, CancerCare Manitoba
Dr. Aaron Marshall, department head and professor of immunology, Max Rady College of Medicine; researcher, Research Institute in Oncology and Hematology, CancerCare Manitoba
Grant: $1,151,326 (five years)
Marshall’s project deals primarily with B lymphocytes, the immune system cells responsible for producing antibodies. The research aims to define the cellular reprogramming signals that either switch on or switch off B lymphocytes and how these networks are altered in chronic autoimmune disease.
 Dr. James Nagy, professor of physiology and pathophysiology, Max Rady College of Medicine
Dr. James Nagy, professor of physiology and pathophysiology, Max Rady College of Medicine
Grant: $898,876 (five years)
Using experimental mouse models, Nagy and the team will determine how spinal neurons, called V0c neurons, contribute to force level control in the limbs. He expects the results will challenge current textbook knowledge on force generation during movement and reveal new concepts on how command signals to motoneurons are converted to desired levels of muscle activity.
 Dr. Zulma Rueda, associate professor of medical microbiology and infectious diseases, Max Rady College of Medicine; Canada Research Chair in Sexually Transmitted Infection – Resistance and Control
Dr. Zulma Rueda, associate professor of medical microbiology and infectious diseases, Max Rady College of Medicine; Canada Research Chair in Sexually Transmitted Infection – Resistance and Control
Grant: $688,501 (four years)
Rueda will lead a study that will generate a comprehensive and systematic understanding of the knowledge, attitudes and practices about HIV and other sexually transmitted and blood-borne infections (STBBI) among people living with HIV and people who face disproportionate risk of acquiring HIV/STBBI (people experiencing houselessness, people who inject drugs) and health and service providers in Manitoba.
 Dr. Tabrez Siddiqui, associate professor of physiology and pathophysiology, Max Rady College of Medicine; researcher, Kleysen Institute for Advanced Medicine, Health Sciences Centre; researcher, Children’s Hospital Research Institute of Manitoba
Dr. Tabrez Siddiqui, associate professor of physiology and pathophysiology, Max Rady College of Medicine; researcher, Kleysen Institute for Advanced Medicine, Health Sciences Centre; researcher, Children’s Hospital Research Institute of Manitoba
Grant: $1,143,676 (five years)
Neurexins are essential proteins that help nerve cells in the brain communicate with each other, and changes in the genes for these proteins can increase the risk of developing autism. Siddiqui’s research highlights the possibility of fixing certain brain communication issues by targeting specific proteins, offering hope for new treatments.
 Dr. Jillian Stobart, assistant professor, College of Pharmacy
Dr. Jillian Stobart, assistant professor, College of Pharmacy
Grant: $944,776 (five years)
Stobart’s project aims to determine how the communication between astrocytes and neurons occurs. This will be the first evidence that astrocytes can change brain circuits responsible for the sense of touch and is important because astrocyte-neuron communication changes in disease. Problems with astrocytes and their communication with neurons could be the missing link in these disorders.
 Dr. Geoffrey Tranmer, associate professor, College of Pharmacy
Dr. Geoffrey Tranmer, associate professor, College of Pharmacy
Grant: $730,576 (five years)
Tranmer and the team plan to create new and improved versions of the ALS drug edaravone and test the drug-like properties of these molecules in test tubes and ALS animal models. This will allow the team to determine and optimize the drug properties of the new ALS drug and will enable them to develop an optimized drug candidate ready for advanced clinical trials.






