International trials of blood thinners in critically ill COVID-19 patients pause due to futility
Three clinical trial platforms working together to test the effects of full doses of anticoagulants (blood thinners) in COVID-19 patients have paused enrollment for one group of patients. Among critically ill COVID-19 patients requiring intensive care unit (ICU) support, therapeutic anticoagulation drugs did not improve outcomes. Enrollment continues for moderately ill hospitalized COVID-19 patients in the trials.
As is normal for clinical trials, these trials are overseen by independent boards that routinely review the data and are composed of experts in ethics, biostatistics, clinical trials, and blood clotting disorders. Informed by the deliberations of these oversight boards, all of the trial sites have paused enrollment of the most critically ill hospitalized patients with COVID-19. A potential for harm in this sub-group could not be excluded. Increased bleeding is a known complication of full-dose anticoagulation. The trials are working urgently to undertake additional analyses which will be made available as soon as possible.
At the recommendation of the oversight boards, patients who do not require ICU care at the time of enrollment will continue to be enrolled in the trial. Whether the use of full-dose compared to low-dose blood thinners leads to better outcomes in hospitalized patients with less severe disease remains a very important question.
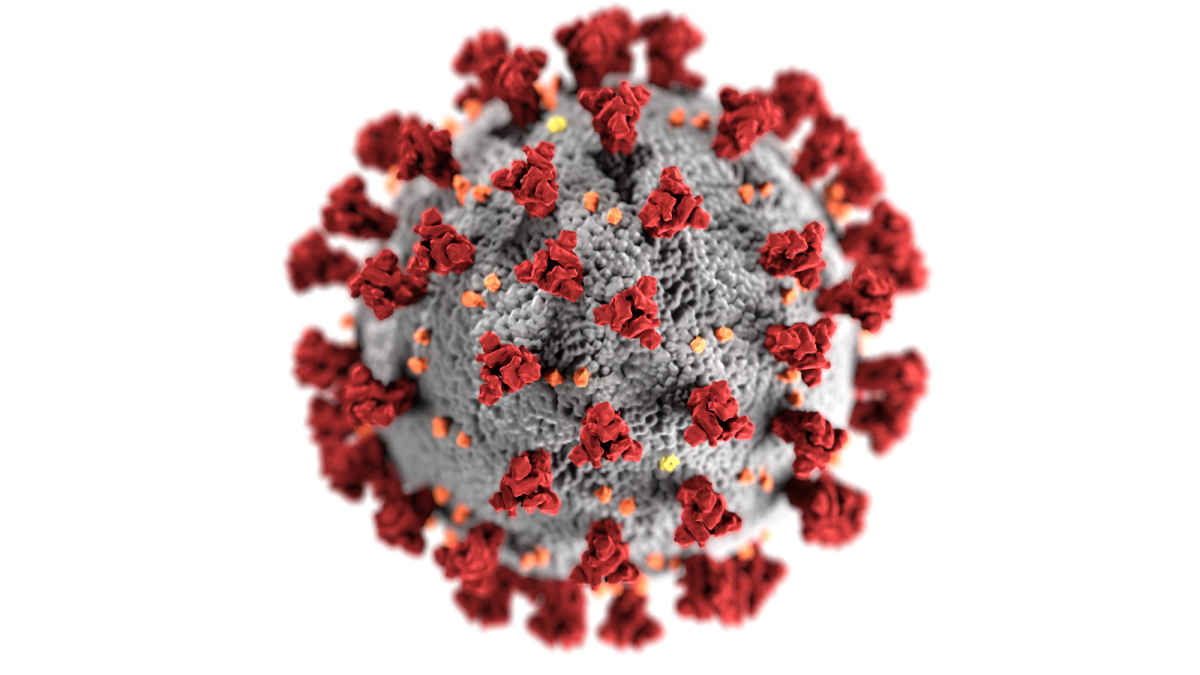
COVID-19 is associated with significant inflammation and clinical and pathologic evidence of widespread blood clots. These trials were launched because clinicians have observed that many patients ill with COVID-19, including those who have died from the disease, formed blood clots throughout their bodies, even in their smallest blood vessels. This unusual clotting can cause multiple health complications, including lung failure, heart attack, and stroke.
“In only our most critically ill patients with COVID-19, all of our trial sites have paused enrollment while we further analyze the data. These results question the benefit of giving full dose anticoagulants routinely in COVID-19 patients who are admitted to an ICU,” said Dr. Ryan Zarychanski, associate professor of medicine at the University of Manitoba and CancerCare Manitoba, a hematologist and critical care physician, who led the harmonization of the three trials.
The multiple-platform, randomized controlled trial (mpRCT) represents an unprecedented collaboration between three international partners. The Randomized, Embedded, Multi-factorial Adaptive Platform Trial for Community-Acquired Pneumonia (REMAP-CAP) Therapeutic Anticoagulation; Accelerating COVID-19 Therapeutic Interventions and Vaccines-4 (ACTIV-4) Antithrombotics Inpatient; and Antithrombotic Therapy to Ameliorate Complications of COVID-19 (ATTACC) are a set of clinical trial platforms spanning five continents with the common goal of testing whether there is a benefit of full doses of blood thinners to treat adults hospitalized for COVID-19 illness on the ward or in the ICU compared to the lower dose used to prevent blood clots in hospitalized patients. To meet the challenge of this pandemic, investigators worldwide joined forces to answer this question as rapidly as possible.
“These results represent an immense collaborative effort involving patients, clinicians, and research staff around the world enabling us to rapidly learn how best to treat Covid-19,” says Dr. Ewan Goligher, assistant professor of medicine, University of Toronto and scientist, Toronto General Hospital Research Institute, University Health Network, and critical care physician. “The strength of the multiplatform clinical trial design enables us to pause in one subset and continue parts of the study.”
The trials are supported by multiple international funding organizations including Canadian Institutes of Health Research (CAN), National Institutes of Health Research (UK), National Health and Medical Research Council (AUS) and the National Institutes of Health (US) and the PREPARE and RECOVER consortia (EU).
In Canada, the collaboration was funded by Canadian Institutes of Health Research, LifeArc Foundation, Research Manitoba, Thistledown Foundation, Province of Ontario and Peter Munk Cardiac Centre at UHN.







Are any studies being done to monitor mild cases? I know hyperviscosity has been observed in patients who didn’t require hospitalization. Will aspirin help these patients? Is this widely recommended?