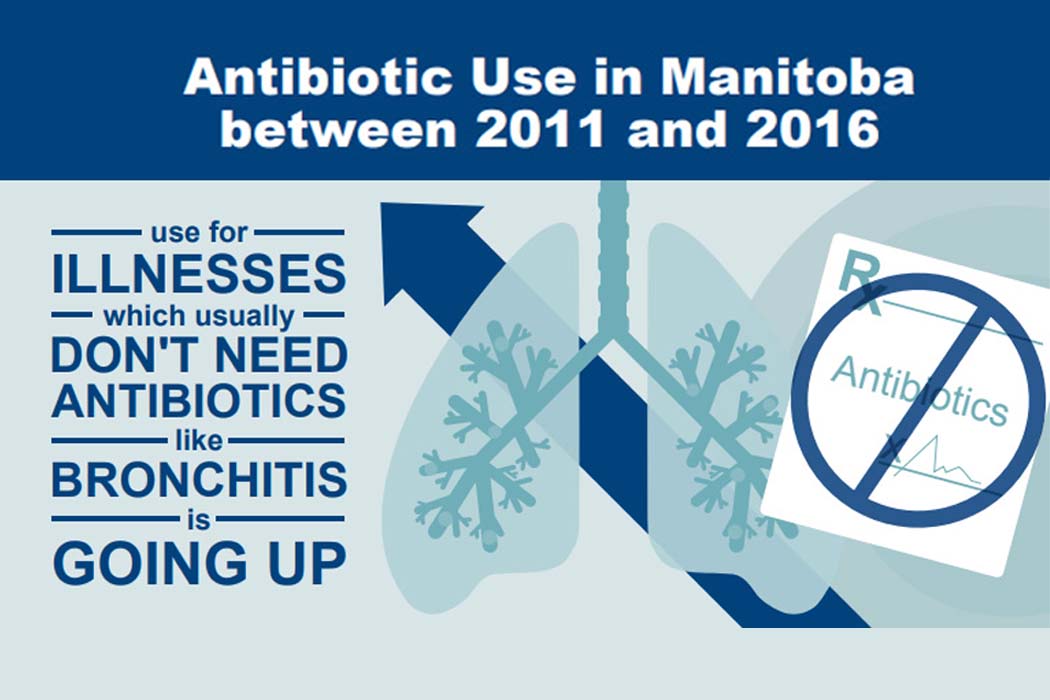
INFOGRAPHIC BY MANITOBA CENTRE FOR HEALTH POLICY
Inappropriate prescribing of antibiotics on the rise in Manitoba: UM study
Manitoba doctors are increasingly prescribing antibiotics for conditions that generally should not be treated with these drugs, a University of Manitoba study has found.
Doctors also frequently prescribe the wrong type of antibiotic, says the study by researchers at the Manitoba Centre for Health Policy in the Rady Faculty of Health Sciences.
The study is the first to measure non-hospital antibiotic prescribing across Manitoba. It looked at antibiotics dispensed at pharmacies from 2011 to 2016.
Doctors prescribed 87 per cent of the antibiotics, with professionals such as dentists, nurse practitioners and pharmacists prescribing the remainder.
The researchers found that 73 per cent of patients with bronchitis (commonly called “chest cold”) were prescribed an antibiotic, even though bronchitis usually does not need this treatment.
Patients with bladder infections were most often prescribed antibiotics from the quinolone class. But these drugs are not recommended for bladder infection because they also kill bacteria that don’t cause the illness.
In treating pneumonia, the wrong type of antibiotic was prescribed for 52 per cent of children under 15 years old. In patients of all ages, ear infection was treated with an inappropriate antibiotic 23 per cent of the time. Throat infection was treated with the wrong choice of antibiotic 30 per cent of the time.
Overall, the rate of dispensing antibiotics for conditions that generally don’t require them – such as acute bronchitis, asthma, cough, allergy-related runny nose and upper respiratory tract infection (common cold) – was significantly higher in most age groups in 2016 than in 2011.
“These findings are alarming,” said Dr. Chelsea Ruth, assistant professor of pediatrics and child health, who co-led the study. “They show that Manitoba physicians are not consistently following Canadian recommendations. This results in an increasing number of unnecessary or poorly chosen antibiotics being prescribed.”
Higher antibiotic use, Ruth said, contributes to the growing worldwide problem of antibiotic resistance, which happens when bacteria are overexposed to a drug and are no longer killed by it. Receiving an unnecessary antibiotic also puts a patient at risk of side effects or adverse reactions, with no benefit.
“Our results indicate that Manitoba needs antibiotic stewardship programs to educate and support prescribers while promoting optimal prescribing practices,” said study co-leader Dr. Sergio Fanella, associate professor of medical microbiology and infectious diseases.
To conduct the study, the researchers analyzed de-identified (anonymous) pharmacy dispensing data, linking antibiotic prescriptions with the diagnostic codes entered by prescribers for illnesses.
Over the five-year study period, the use of antibiotics rose at a faster rate than population growth. Antibiotic use was highest among seniors and children under five.
Older doctors, physicians who saw more patients on a daily basis and those in the Prairie Mountain Health region were more likely to prescribe antibiotics for conditions that should not be treated with these drugs.
Patients who saw their regular doctor had less antibiotic use and were less likely to be prescribed an inappropriate antibiotic.
“This highlights the importance of doctors having an ongoing relationship with patients and knowing their health history,” said Fanella.
The researchers’ recommendations include:
- Patients should try to see their regular doctor, and the health-care system should remove barriers to ensure that everyone has access to a consistent primary care provider.
- Antibiotic stewardship programs should be established, particularly focusing on conditions with the highest rates of antibiotic misuse. These include pneumonia and bronchitis in adults and pneumonia, sore throat and ear infections in children.
- Data should be used to provide individual prescribers with regular feedback on their antibiotic prescribing in comparison to that of their peers. This is an evidence-supported strategy to improve antibiotic use.
View the study infographic, summary and full report.






