Breaking boundaries in pediatric cancer:
Study reveals a path towards targeted treatment for medulloblastoma
A newly published study on childhood brain cancer offers hope for more targeted treatment with fewer side effects.
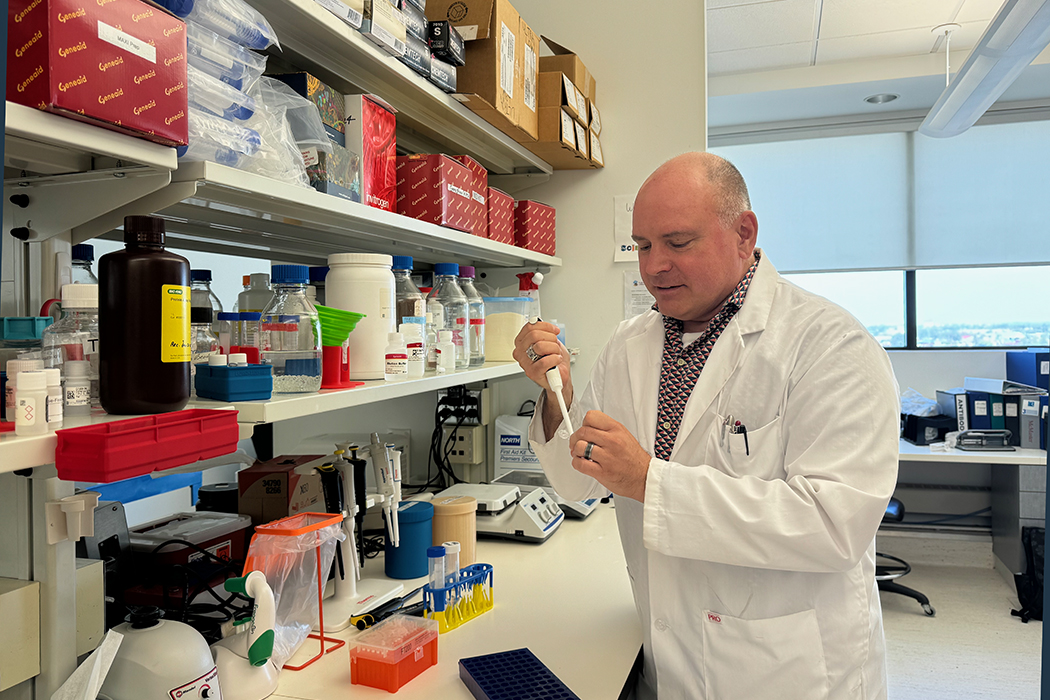
The study, published in Nature Cell Biology, was the work of a high-powered team including Dr. Brad Doble, associate professor of pediatrics and child health at the Max Rady College of Medicine and the Bihler Chair in Stem Cell Research, and colleagues Michael Taylor and Tamra Ogilvie at Baylor College of Medicine, Houston, Texas.
Multiple UM labs were also supported the research including Central Animal Care Services, the Small Animal and Materials Imaging Core Facility and the Manitoba Centre for Proteomics and Systems Biology.
“The type of brain cancer I’m studying is called medulloblastoma,” explained Doble. “It’s rare but is the most prevalent of pediatric brain cancers, accounting for nearly 20 per cent of all pediatric cancers.”
Medulloblastoma occurs in the cerebellum, a part of the brain located at the base of the skull, responsible for co-ordination and motor functions. Symptoms can include intense headaches, balance problems, difficulty with movement, nausea, vomiting and changes in behavior or personality.
One of the critical challenges in treating medulloblastoma is the current approach, which is broad and aggressive. “It involves whole brain and spinal cord irradiation along with chemotherapy, which has devastating side effects in children whose brains are still developing,” said Doble.
Historically, these tumours were categorized based on their appearance under a microscope, but now, with advances in whole genome sequencing, four main molecular subgroups have been identified.
“This is important because all subgroups, despite their molecular differences, have been treated the same way,” he said.
Doble’s lab, however, is working on changing this approach by developing targeted therapies that consider the unique molecular characteristics of each subgroup.
“This study focuses on Group 3 medulloblastoma, which, despite aggressive treatment, has a five-year survival rate of only about 60 per cent,” he noted, adding previous studies have reported on the significant role OTX2 plays in Group 3 medulloblastoma.
OTX2 is a protein that acts as a transcription factor, which means it helps regulate which genes are turned on or off in cells. In the context of Group 3 medulloblastoma, OTX2 has been found to play a crucial role in the development of the tumour.
Doble and his colleagues investigated how OTX2 interacts with other proteins, specifically RNA splicing factors.
RNA splicing is a process where segments of RNA are cut out and reconnected to create a final messenger RNA (mRNA) that can be translated into a protein. Doble and his team’s research uncovered that OTX2 regulates RNA splicing in a way that promotes tumour growth.
“This was a groundbreaking finding,” Doble said. “In mice engrafted with human Group 3 medulloblastoma tumours, treatments that interfered with this RNA splicing pathway successfully reduced tumour size.”
The implications of this discovery are profound, said Doble. “It opens up a new avenue for treatments,” he said. “Instead of using broad, toxic treatments, we’re moving towards a more precise, less harmful approach. This could significantly improve the quality of life for children undergoing treatment.”






