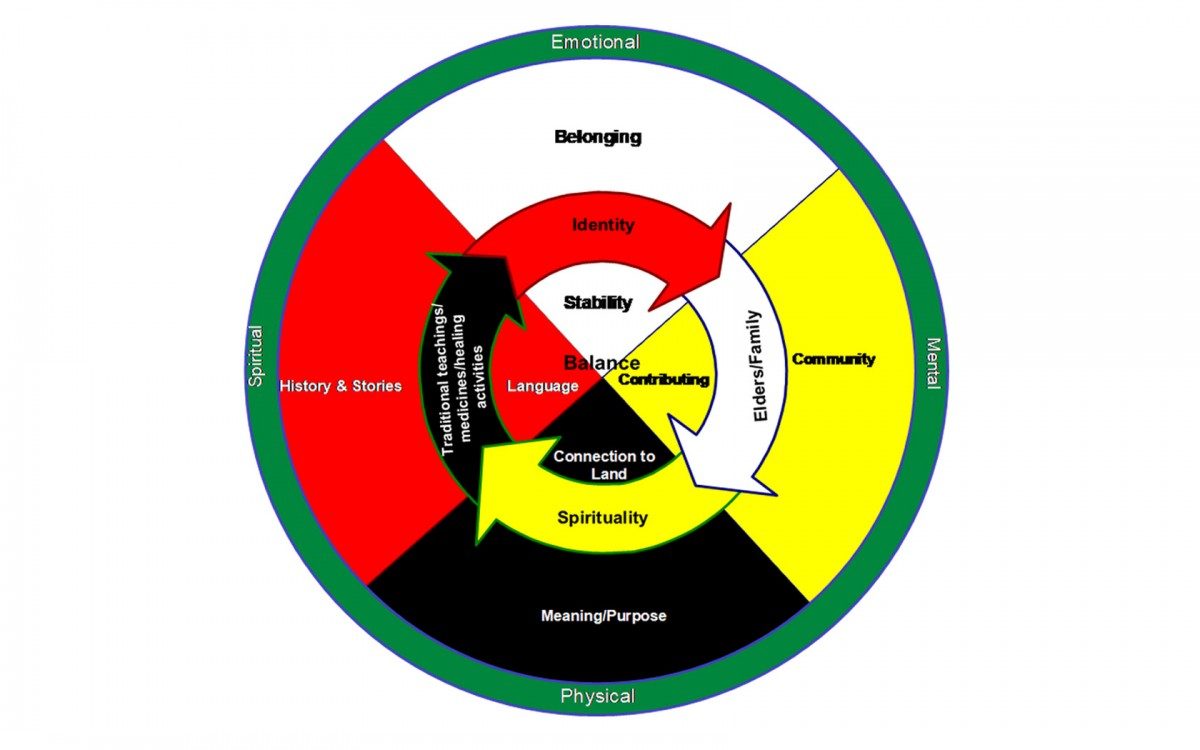
TRADITIONAL STRATEGIES FOR MENTAL HEALTH ARE SEEN AS INTERCONNECTED ON THE MEDICINE WHEEL.
Look to the medicine wheel for mental health, Elders advise in First Nations study
The traditional medicine wheel, symbolizing balance and interconnection, can serve as a framework for improving the mental well-being of First Nations people in Manitoba.
That’s the key recommendation from a mental-health study conducted by eight First Nations communities in partnership with the First Nations Health and Social Secretariat of Manitoba (FNHSSM) and researchers from the University of Manitoba.
“Traditional teachings have to come back in order [for us] to know who we are and how to balance ourselves,” said an Elder participant in the study. “We need to go back to having the mind, the body and the soul reconnect.”
The eight communities, representing all regions of Manitoba and four languages (Ininiwak-Cree, Dakota, Dene and Ojibway/Anishinabe) have high rates of anxiety, depression and suicide that amount to a mental health crisis, the study says.
The study, part of a larger health research project involving the eight communities, was conducted between 2014 and 2016. Funded by the Canadian Institutes of Health Research, it consisted of in-depth interviews or focus groups with 61 Elders and Knowledge Keepers, some of whom are also health-care workers. The interviews were conducted by members of the communities.
Titled Looking back, moving forward: a culture-based framework to promote mental well-being in Manitoba First Nations communities, the study was published online in December 2018 by the International Journal of Culture and Mental Health.
Taking a strength-based approach, the study aimed to describe culture-based practices that are effective in supporting mental health.
“What the Elders gave us is a call to action,” says the study’s lead author, Dr. Grace Kyoon-Achan, a former post-doctoral research fellow in community health sciences at the Max Rady College of Medicine in the Rady Faculty of Health Sciences.
“The biomedical model of treating mental illness is compartmentalized. The medicine wheel framework is holistic. You treat the whole person, within the family and within the community. You support the person in achieving balance in their emotional, physical, spiritual and mental health.”
The Elders identified strategies for mental wellness such as participating in and contributing to the community; finding a sense of meaning and purpose; taking part in spiritual activities such as sweats, ceremonies and round dances; connecting with the land; and gaining knowledge and strength from sharing histories and stories.
A strong theme was that a sense of identity within the community creates feelings of belonging that foster health. “Relationships create co-operative energy for dealing with illness,” the study says.
Ties to the land in one’s home community are powerful for mental health, the Elders said. “When your soul is sick, what you need is not a pill, it’s to go back into that place of connection to family, to homeland, to knowing who you are,” says Kyoon-Achan.
“A big cause of mental illness is dislocation,” says Wanda Philips-Beck, an Anishinabe nurse research manager with FNHSSM and a U of M PhD student who took a leadership role in the study.
“Land-based forms of healing are legitimate. For example, a program to take at-risk youth out to build a lodge and learn to harvest animals in a respectful way teaches them how to live in community, work as a team and develop relationships. That strengthens mental well-being.”
The community-led study included researchers from the U of M department of family medicine and Ongomiizwin – Research, as well as FNHSSM. The published study recommends funding for mental wellness programs based on the medicine wheel model.
Kyoon-Achan and Philips-Beck say such programs are not intended to replace biomedical services, such as psychiatry, but to address the holistic needs that standard medical approaches overlook.
“If you’re a health-care professional, see yourself as one piece of the puzzle,” says Kyoon-Achan. “As you support a First Nations patient, recognize the whole person. Ask questions to learn what else that patient needs on their healing journey.”
Be informed about ways to connect patients to the circle that surrounds them, adds Philips-Beck. “Be aware of resources and supports, and how to refer clients to that network of care, including wise Elders and teachers.”






