Line of Fire
Fall 2018
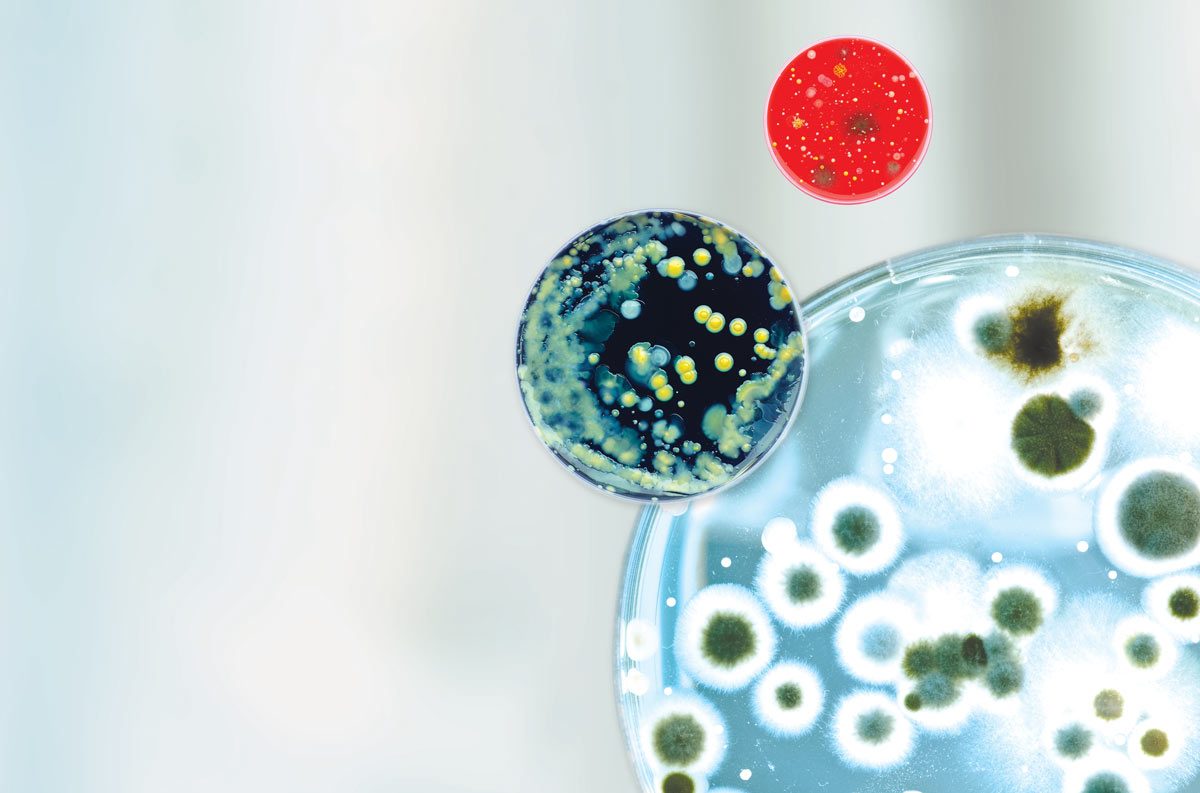
Carmine Slipski is one of the newest recruits in a 75,000-year-old fight: humans versus bacteria.
For the past seven decades, we’ve enjoyed an advantage thanks to antimicrobials. Now, bacteria have figured out our game plan, and turned our best course of action into our biggest weakness.
“We’ve been taught to fear bacteria in our everyday lives, so we’ve been abusing antimicrobials absolutely everywhere,” explains Slipski [BSc(Maj)/15], a PhD candidate in medical microbiology and infectious diseases at the U of M’s Bannatyne campus. “It’s not just overprescribing in clinics. They are in our fabric softener, toothpaste, hand soap and makeup. In Canada, 80 per cent of antimicrobial usage is in livestock.”
We’ve been so reckless in our attack that bacteria have developed antimicrobial resistance to the point that some superbugs are near indestructible. The World Health Organization (WHO) warns that we are rapidly approaching a post-antibiotic era where a small cut could be deadly, and routine dental work, a major risk. Already, 23,000 people in the United States die every year from antibiotic-resistant infections. That number is expected to hit 10 million worldwide by 2050.
Graduate students bring much-needed muscle to the frontlines.
“Antimicrobial resistance does keep me up some nights,” Slipski admits. “But I feel more at ease knowing that some of the brightest minds in the world are working at this problem. Winnipeg is a hub for the study of infectious diseases. There are amazing ideas in the pipeline.”
Some of those ideas are his—Slipski studies efflux pumps in search of ways to overcome bacteria’s seemingly impenetrable armour.
“These are structures in the cell wall that recognize antimicrobials with lock-and-key specificity and pump them out before they take effect,” he explains. “If we can understand the mechanics of how they work, we can use this information to make new antimicrobials more effective.”
At the Fort Garry campus, another graduate student—Rachel Nickel [BSc(Hons)/16]—is looking at new ammunition: topical biocide.
Developed by professor Song Liu in the department of medical microbiology, this potential solution has a significant edge over antibiotics: biocides don’t target specific sites on cells, making it difficult for bacteria to develop resistance. The challenge is ensuring friendly host cells aren’t killed in the process.
“By coating magnetic nanoparticles with biocide, we have a system that we can apply directly to an infection and later remove using an external magnetic field,” she explains. “We’ve shown that we can kill 100 per cent of superbugs P. aeruginosa and MRSA in two hours with minimal impact on human cells.”
Promising results like these have George Zhanel [BSc(Pharm)/84, PhD/94], director of the Canadian Antimicrobial Resistance Alliance, confident it’s not “all doom and gloom.” Rather, he says, the U of M is making novel advances because researchers use the multidisciplinary collaborative approach known internationally as One Health.
“Antimicrobial resistance is a multi-system problem. It’s not just in hospitals. It’s in the community, agriculture, aquaculture, vet medicine. So we try to see where the synergies and overlaps are. There’s tremendous collaboration between university departments, and then we also collaborate with the National Microbiology Laboratory, and other health centres. That sets us apart because other institutions don’t do that.”
The result of this team effort is a stockpile of new weapons and tactics still in development.
Zhanel, a researcher in medical microbiology, has partnered with Frank Schweizer in chemistry to create a hybrid antibiotic with twice the fighting power. In addition to biocide, Lui is finding ways to infuse health-care textiles—like surgical scrubs, lab coats and bandages—with bacteria-killing chlorine bleach. Pavel Dibrov in microbiology and Grant Pierce [PhD/83] in physiology and pathophysiology made headlines last year when they developed a new drug that combats two of the WHO’s “priority pathogens,” P. aeruginosa and Neisseria gonorrhoeae.
If antimicrobials have taught us anything, however, it’s that none of these approaches will, or should, become the catch-all solution to this age-old problem. We need to continue finding different ways to strike at bacteria’s defences, and these discoveries will come from next-generation scientists like Slipski and Nickel, says Zhanel.
“Bacteria have been around for billions of years, through everything: ice age, fires, famine, disease and antibiotics. There’s no question this problem will continue so we need to be mentoring the best and brightest for the future. Graduate students are the future.”
GRADUATE STUDENT SUPPORT AT THE U OF M
 Dr. Bonnie Buhler Graduate Scholarships in Music
Dr. Bonnie Buhler Graduate Scholarships in Music  Marjorie Blankstein Emergency Graduate Student Bursary for Peace and Conflict Studies
Marjorie Blankstein Emergency Graduate Student Bursary for Peace and Conflict Studies University of Manitoba Alumni Association Graduate Fellowship
University of Manitoba Alumni Association Graduate Fellowship
Our graduate students are the primary workforce of our research engine, and attracting them is a highly competitive global business. If we are to continue our renowned efforts in areas like antimicrobial resistance, we must invest in these bright minds.
To support the next generation of innovators through the Front and Centre campaign, visit give.umanitoba.ca